By Marie Y. Lemelle
Contributing Writer
The Centers for Disease Control and Prevention reported that 60 million people in the U.S. have received one dose of the vaccine and more than 31 million have been fully vaccinated. On the average about 2.2 million people are getting vaccinated daily.
While that means following precautions can be a little more relaxed for those who are fully vaccinated, the CDC warns that millions more need to be vaccinated before the current COVID-19 precautions can be lifted due to new variants and surges in travel.
The CDC makes recommendations for vaccine eligibility requirements and each state makes it own plans. Alaska is the first state to remove the eligibility requirements making it available to anyone over 16 years old as long as they live or work in the state. In many states, the vaccine appointments are going unclaimed. Los Angeles County’s criteria is listed on the California Department of Public Health’s MyTurn.com site.
It is important to note that people with underlying medical conditions, especially those with diabetes coupled with an eye disease are at a greater risk for intubation if infected with the coronavirus. In fact, studies have shown that patients hospitalized for diabetic retinopathy and COVID-19 are five times more likely to need intubation and put on a ventilator to be able to breathe.
A study conducted by Reuters found that 40% of deaths out of 100,000 COVID-19 affected people had diabetes with eye disease known as diabetic retinopathy. According to the National Eye Institute, about 40% of Americans with diabetes have some stage of diabetic retinopathy and 40% of patients who are at high risk for vision loss did not visit an eye doctor or receive an eye exam in the last year.
The risk for diabetic retinopathy is the presence of diabetes. For that reason, the American Academies of Ophthalmology and Family Practice recommend that all diabetic patients should be screened for retinopathy at least once a year. Other risk factors include diabetes with a history of hypertension, hyperlipidemia, cardiovascular disease and tobacco use.
COVID-19 is related to diabetic retinopathy indirectly.
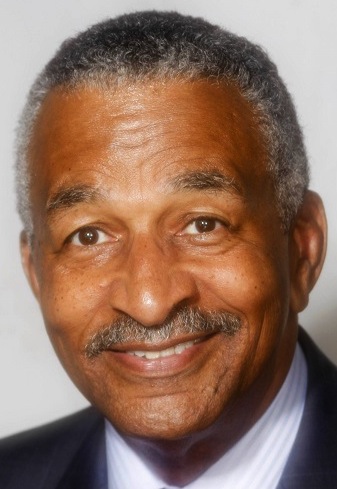
“With the pandemic, people have become less active and likely have poorer diets related to access, stress and isolation,” said Dr. Keith A. Warren, a board-certified ophthalmologist who specializes in diseases and surgery of the retina and vitreous. “Other conditions like hypertension, high cholesterol and tobacco use are also likely to worsen. In addition, if they become ill, the stress of any illness increases the blood sugar which creates a bad cycle.”
Warren who is an active member of the American Academy of Ophthalmology, the Retina Society, the American Society of Retinal Specialists, the American Society of Cataract and Refractive Surgery and the Sports Ophthalmology Society of the Americas further explained diabetic retinopathy as a disease of the retina directly related to poor control of the blood sugar.
“The high blood sugar damages blood vessels in all of the body’s organs including the eye,” he said. “Those damaged vessels leak their contents into the tissue and that causes the tissue to malfunction, in the case of the eye, it results in loss of vision.”
There is nonproliferative diabetic retinopathy and proliferative diabetic retinopathy.
Nonproliferative diabetic retinopathy is the earliest form of retinopathy and is characterized by the changes described above (blood, fluid or fatty tissue). If that leakage occurs in the center of the retina (macula), the vision may be impaired and require treatment.
Proliferative is the more advanced and dangerous form of retinopathy. In this form, the damaged blood vessels close off and the blood flow is halted. The areas of the retina are starving for nutrients and oxygen releases a chemical that causes new, abnormal, blood vessels to grow or proliferate.
The abnormal vessels tend to bleed easily and turn to scar tissue. Untreated, the process leads to severe vision loss in 25% of these patients and is the leading cause of blindness in people between the ages of 25-65.
People can be screened for retinopathy by telemedicine.
“It requires a camera that can photograph the retina looking for the evidence of damaged blood vessels that were previously mentioned,” Warren said. “The photographs can be taken through an undilated pupil and transmitted to a doctor who is screening for those changes. When those changes are noted, the patient can be referred to an ophthalmologist for further evaluation and treatment if necessary.”
Treatment for diabetic retinopathy depends on the type and extent of the retinopathy present. The mainstay of treatment is patients improving the control of their blood sugar, blood pressure and lipids.
“With nonproliferative retinopathy associated with swelling in the center of the retina, injections of medication directly into the eye have been shown to be very effect in reducing the leakage and improving the vision,” Warren said. “In proliferative diabetic retinopathy, any high-risk abnormal blood vessel growth should be treated with lasers, which can cause those vessels to melt away.”
Some patients also can be effectively treated with injections into the eye. For patients with more advanced disease, they require complex eye surgery known as vitrectomy to remove any bleeding or scar tissue.
“There outcomes are more guarded depending on the extent of disease present,” Warren said. “The best treatment is control of the blood sugar, reducing the other risk factors and regular screening exams.”
Marie Y. Lemelle is the founder of www.platinumstarpr.com and a film producer. She can be reached at MarieLemelle@platinumstarpr.com. Follow her on Instagram @platinumstarpr.