By Marie Y. Lemelle, Contributing Writer
Face masks have become part of our daily attire and protection against the spread of COVID-19. Medical experts predict that it may be a year before we can quit wearing a face covering in public.
Millions of masks are being made and sold around the world, whether they be a three-ply cloth or copper or silver infused. There is no question that for an individual at a high risk of being exposed to the virus, an N95 mask is your best bet. The bigger question is whether the N95 purchased on the street or online is real or counterfeit.
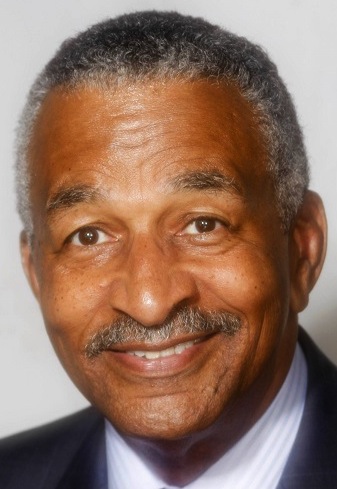
Frontline medical professionals like Dr. Nicholas Caputo, associate chief of the Department of Emergency Medicine at NYC H+H/Lincoln Medical Center is one of thousands of emergency room doctors who wear a medical mask long past an 8 to 12-hour shift to help resuscitate patients, and make sure the oncoming teams are not too overwhelmed.
Caputo is also an attending emergency physician at the Columbia University Irving Medical Center/New York Presbyterian Hospital. As an emergency physician and member of the Sollis Health Medical Concierge Service, Caputo has had a long tenure of work in underserved communities and medical research specifically focused on the socioeconomic disparities in medical care, which disproportionately affect Black and indigenous people of color across the nation. He talked about the authenticity of medical face masks and positive outcomes of COVID-19 cases because of wearing face masks properly.
ML: What are the ways in which we can determine authenticity between real and fake N95 masks?
NC: The Centers for Disease Control and Prevention identifies several signs that a respirator may be counterfeit: no markings at all on the filtering face piece respirator; no approval number on filtering face piece respirator or headband; no NIOSH markings, NIOSH spelled incorrectly, presence of decorative fabric or other decorative add-ons (e.g., sequins), claims for the of approval for children (NIOSH does not approve any type of respiratory protection for children), and filtering face piece respirator has ear loops instead of headbands. The National Institute of Occupational Safety and Health (NIOSH) also provides a list to determine authenticity based on specific markings, labelling, approval numbers, etc.
ML: What are best practices for wearing and cleaning masks?
NC: Ideally, N95 mask is a single-use mask worn in high-risk exposure situations. In the hospital, the situations would be in interactions with patients that are known to have or there is a high suspicion of infection that is spread by aerosolization, i.e. droplets. Usually, aerosolization is caused by coughing, sneezing, even talking in the natural environment. Aerosolization can be significantly increased by certain procedures, such as non-invasive ventilation, endotracheal intubation, bronchoscopy or the obtainment of nasopharyngeal samples (swabs).
Check with the manufacturer regarding cleaning these masks as there are no real concrete guidelines for how to clean/purify a soiled or used N95 mask. Proper fitting of an N95 requires a fit test to determine whether there are any air leaks. Leaks can be caused by wearing a mask that is not the proper size for the individual, if the individual has facial hair or if they fail to mold the nasal bar appropriately to the contours of their face.
If wearing a regular surgical mask or bandana or other type of cloth mask (which is suitable for everyday use outside the clinical environment), these masks are usually intended to prevent the wearer from spreading aerosols as opposed to filtering the air one is breathing in.
ML: What have you witnessed because people were not wearing masks properly?
NC: In March, people were coming into the ER in droves because nobody was wearing masks or socially distancing. When policies were put in place by the federal and local government, we saw a reduction of cases in New York by the end of April with a steady decrease in May through the present. Not wearing a mask properly puts everyone at greater risk for transmission and infection, as does congregating in large crowds.
ML: How has mask wearing requirements in the ER and OR changed from six months ago at the beginning of the pandemic to now?
NC: The biggest change has been the requirement to wear personal protection equipment (PPE) (i.e. masks, face shield, eye protection, gowns, gloves) throughout work shifts. Prior to COVID-19, wearing PPE was only done when in direct contact with a highly suspected or known infected patient and isolation precautions. ER doctors generally work in shifts (usually 8, 10- or 12-hour shifts with 12 hours being the most common shift). During the pandemic surge, wearing masks for long periods of time caused bruising and indention on our faces because our shifts were non-stop with little to no time to take our masks off.
Marie Y. Lemelle is the founder of www.platinumstarpr.com and a film producer. She can be reached at MarieLemelle@platinumstarpr.com. Follow her on Instagram @platinumstarpr.