Rx REPORT
By Marie Y. Lemelle
Contributing Writer
Post-traumatic stress disorder is a growing mental health problem. In the U.S., more than 7 million people over 18 suffer from PTSD and those numbers are increasing due to COVID-19, social and racial injustices and the fear about the future of the American government. It is estimated that 200 million or more people suffer from PTSD worldwide.
So, what is PTSD? One of the most common definitions that people associate with the condition is that it generally affects active military service members and veterans who used to be referred to as “shell shocked.” Acts of war was the common foundation of trauma experienced from the front lines and being bombarded with gunfire and loud explosives and, in numerous cases, death. Interestingly enough, a 1988 study reported that almost a million of the 3.14 million men who served in Vietnam had suffered PTSD at some point even though only 20% of veterans had been assigned to combat units.
In fact, research discovered that there are five different subcategories of PTSD that require different treatment methods. Normal stress response usually occurs prior to full-blown PTSD as a result of events such as accidents, injuries, illnesses, surgeries and other sources of tension and stress.
Acute stress disorder can occur in people who have been exposed to what is or what feels like a life-threatening event like a natural disaster, loss of loved ones, loss of a job or risk of death. That disorder can develop into PTSD.
Uncomplicated PTSD is the cause of one major traumatic event, as opposed to multiple events. Symptoms include avoidance of trauma reminders, nightmares, flashbacks to the event, irritability, mood changes and changes in relationships.
Complex PTSD is the result of suffering multiple traumatic events such as abuse or domestic violence cases, repeated exposure to war or community violence, or sudden loss.
Comorbid PTSD is based on co-occurring disorders and often coupled with substance abuse issues. Many people who suffer from PTSD try to treat it by self-medication and other destructive behavior to numb the pain.
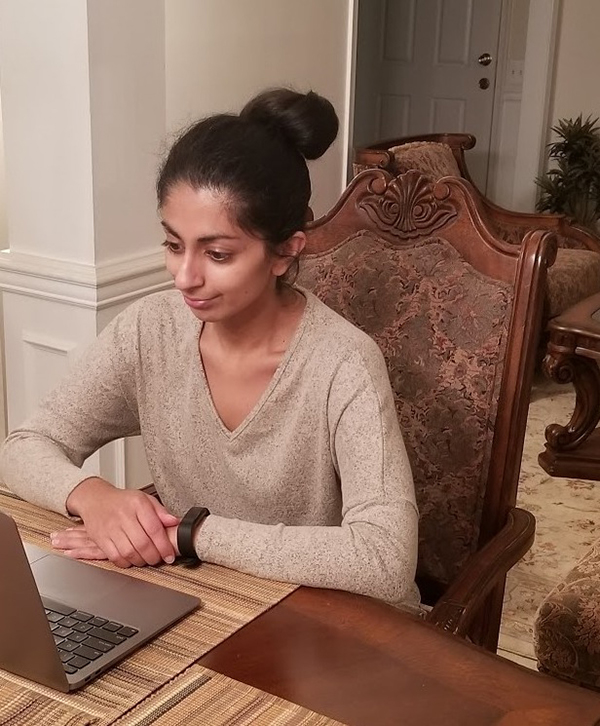
Medical social worker and clinician Silvi Saxena, a contributor to Choosing Therapy, has worked with patients of all ages with a wide variety of complex medical and psychosocial concerns. Her specialties include PTSD (veterans), PTSD (trauma related to personal injury/traumatic event), and PTSD (survivorship). Saxena talks about how COVID-19 impacts people with PTSD and how the pandemic has increased PTSD in the world.
ML: What is the impact of COVID-19 on the PTSD population?
SS: The impact of social isolation as a result of COVID-19 can worsen PTSD symptoms and those who already struggle with a PTSD diagnosis. The isolation can often feel similar to previous feelings of isolation and result in depression and fear. Fear, in this case, is fear of getting sick or dying from COVID-19. However, the fear can be presented as fear experienced in the past. As a result, patients with PTSD tend to have more walls up during the pandemic as a protective mechanism.
ML: What are the estimated statistics of PTSD sufferers pre and post COVID-19?
SS: According to the American Psychological Association, PTSD impacts 3.5 to 4% of the American population every year pre-COVID-19. In veterans, that number is much higher, however; underreported. Post-COVID-19, those statistics are still changing as the pandemic continues on.
What we do know is that right now, 50% of the American population has reported increased feelings of anxiety, depression, and distress from the on-going COVID-19 pandemic, financial strains, social isolation, and job insecurity.
ML: What is the recommended coping mechanism?
SS: The majority of patients with PTSD tend to cope well by participating in meaningful activities, spending time with close loved ones, and practicing good mental health care and wellness. During the pandemic, many don’t have access to mental health services as a result of closures and teletherapy not being widely accessible.
Additionally, closures such as adult day care centers and senior centers make socialization a challenge, especially those without a strong family support system. Support groups can be found through the Veterans Administration and local community behavioral health organizations.
ML: What are the signs of someone affected with PTSD?
SS: Some signs are anxiety, trouble sleeping, nightmares, feeling unsafe/afraid, depression, anger, feeling withdrawn, triggered by specific noises or colors. People can also experience dissociative thinking and separation of their mind and their body.
ML: Are there recommended treatments?
SS: Yes. There are several psychotherapies that are effective for PTSD. Eye movement desensitization and processing is an individual psychotherapy that can help patients process upsetting memories, thoughts, and feelings related to the trauma. The patient holds the memory in their mind while paying attention to a back-and-forth movement or sound until distress decreases.
Cognitive processing therapy is a trauma-focused psychotherapy that helps people recognize how trauma has changed their view about themselves, others, and the world. CPT teaches people to recognize the negative thoughts that are created by the trauma and consider a more balanced perspective.
Prolonged exposure therapy is a psychotherapy treatment for people who, after a traumatic event, experience unwanted thoughts, disturbing nightmares, feelings of hopelessness, depression, and hypervigilance. PET is based on associative learning theory to help decrease the unwanted traumatic reminders.
For more information, contact the National Center for PTSD at (802) 296-6300. Veterans can find help at the Veterans Crisis Line at (800) 273-8255 (Press 1).
Marie Y. Lemelle is the founder of www.platinumstarpr.com and a film producer. She can be reached at MarieLemelle@platinumstarpr.com. Follow her on Instagram @platinumstarpr.