Rx Report
By Marie Y. Lemelle
Contributing Writer
These days, most of us are living in some level of fear: COVID-19 infection, self-isolation, homelessness, incarceration; lack or the expense of health services; and food insecurities.
For someone with a mental illness or addiction, fear of this “new normal” is magnified. Social distancing within communities has also decreased the likelihood of observed overdoses.
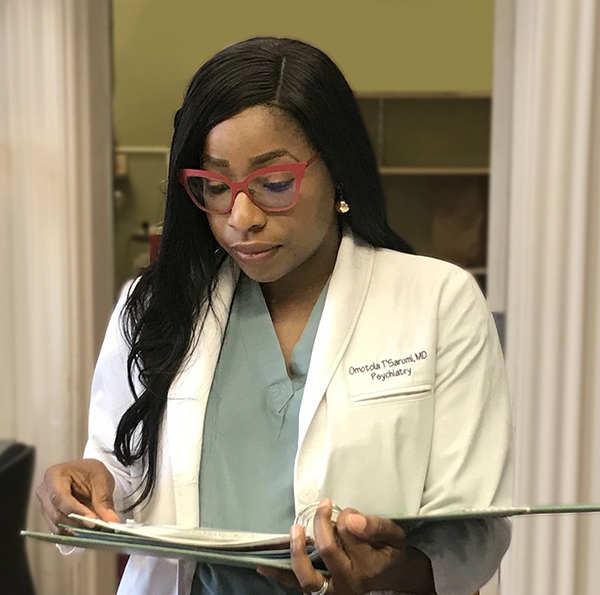
Dr. Tola T’Sarumi, a licensed psychiatrist and emotional wellness strategist, is passionate about women’s issues and overcoming the stigmas associated with mental illness, addiction, substance abuse and suicide.
“Stigma is a significant problem that remains a barrier to accessing and utilizing care by marginalized groups,” said Dr. T’Sarumi, a recipient of numerous awards for her work on “Alcohol Use Disorder,” “Physician Suicide: The Silent Epidemic” and “Synthetic Cannabinoid Use.” “Stigmatization can be conceptualized as someone being labeled, stereotyped, socially excluded, and discriminated against.”
T’Sarumi says, “Terms like ‘addict,’ ‘alcoholic,’ ‘pot or crack head,’ ‘junkie and ‘loser’ are terms that make it even worse for individuals more so for the health care professional.”
She knows firsthand about stigmatism. Her uncle had a substance abuse problem. While family and friends tried to intervene, he was in denial and threatened anyone who tried to help him. He died at the age of 55.
“Stigma causes delay or avoidance in seeking health care treatment, which worsens disease progression, reduces treatment compliance, and further increases the risk of relapse,” she said.
To help shed a light of how to cope with problems that can indirectly or directly affect the population, cause a relapse, or trigger hidden issues, Dr. T’Sarumi answered a few questions.
ML: Excessive alcohol use leads to more than 93,000 deaths each year in the United States. Talk about the link between COVID-19 and how alcohol weakens your body’s ability to fight infections.
TT: During this pandemic, we have seen a substantial increase in substance use disorder from stress, uncertainties, financial impacts and social isolation. Individuals with substance use disorder (SUDs) commonly experience respiratory and cardiovascular disorders, including hypertension and COPD, and have suppressed immunity, making them vulnerable to COVID-19.
Alcohol use affects all organs in the body from short term to long-term consumption and every alcoholic drink has a way of adversely affecting one’s health. Excessive alcohol consumption can lead to changes in gene expression and affect immunity and its ability to fight infection. Studies have shown that alcohol-induced inflammatory cytokine release could expose COVID-19 patients to excessive inflammatory responses. Alcohol use raises the risk of developing acute respiratory distress syndrome (ARDS), one of COVID-19’s severest complications.
ML: What is the high-risk of COVID-19 for people who smoke or vape, or who have a SUD?
TT: Smoking has been described as an adverse prognostic COVID-19 predictor. Apart from conventional risks to cardiopulmonary health raised by smoking, the leading risk factor associated with COVID-19 is increased expression of type 2 angiotensin-converting enzyme (ACE) among smokers. Therefore, the nicotinic pathway mediated overexpression of ACE-2, the putative SARS-CoV2 receptor may be associated with increased virion intake. Patients with weakened lung conditions are at a higher risk for COVID-19. Other substances such as alcohol, opioids and methamphetamine function through the brain and immune system to indirectly affect the respiratory system.
ML: What is the indirect or direct effect on the physiology of our bodies from drugs and alcohol?
TT: Drug use can have a broad array of direct and indirect consequences and sometimes the effect of this depends upon the specific drug or drugs being used, how they are used, how much is used, the health of the person and other factors. Alcohol interferes with the signaling mechanisms of the brain, which can change the way the brain looks and works. Drinking a lot or too much over a long time or a single occasion can harm the heart, liver, pancreas and the immune system. Chronic drinkers have a higher chance of developing diseases such as pneumonia and tuberculosis than those who don’t.
Opioid use disorder can slow breathing rate thereby decreasing oxygenation in the blood. Methamphetamine may contribute to pulmonary hypertension. One of the most important causes of pulmonary edema are cardiac pathologies, which reduces the lung capacity due to fluid collection in the lungs and constriction of blood vessels severely complicated by COVID-19 symptoms.
ML: How can Individuals who are fighting to stop using drugs or are in recovery cope during the pandemic?
TT: The pandemic has brought a whole new way of living and adjustments. SUD is no different. Addiction tends to be a disease of isolation and the struggle persists for individuals during this pandemic.
Treatment is available. Recovering facilities and rehab programs are still open. If you have an alcohol use disorder and are experiencing withdrawal, go to your local emergency room or urgent care for help. Peer support groups counseling, therapy sessions, and sponsors are available virtually.
ML: What do friends and family need to know and how can they help?
TT: Addiction is a difficult challenge for anyone. Family and friends should prepare to handle the challenges of the disease. Educate yourself on the disease. Know the signs and symptoms, such as, appears intoxicated more often, stealing, lying, withdrawal symptoms from the lack of access to a drug, and hygiene and appearance negligence. Seek help from physicians, counselors and programs that specialize in the treatment of SUD.
ML: What lessons learned have you seen from your work that we should keep in mind now during COVID-19?
TT: As an addiction psychiatrist, I had to adjust to the pandemic and offer health care in a different way. Rapid changes in regulations and guidance made during COVID-19 response has played a significant role in stabilizing the medical community and the general population. I am able to initiate opioid treatments without physically seeing them because of the Ryan Haight Act. Previously a physician was prevented from prescribing meds like Buprenorphine and other controlled addiction treatment medications to patients only seen virtually.
Marie Y. Lemelle is the founder of www.platinumstarpr.com and a film producer. She can be reached at MarieLemelle@platinumstarpr.com. Follow her on Instagram @platinumstarpr.