By Tia Delaney-Stewart
Guest Columnist
Advocating for those who often don’t have the capability to advocate for themselves is a humbling responsibility.
As a nurse, I value the role of being the voice of those who are often overlooked and underserved; and I know that there are many community leaders like me, who have powerful voices to deliver messages of education and awareness, which can ultimately lead to actions of reform and change.
That being said, I’d like to share some insight on how associated discrimination, racism and negative biases create health care access barriers for diverse populations living with Alzheimer’s disease and other dementias. These barriers impede many families of color from the opportunity of receiving an early diagnosis, which directly affects their ability to effectively plan for the physical, financial and emotional responsibilities that they and their families will eventually face.
More importantly, their unawareness also impedes them from taking the necessary steps to assist their loved ones in managing this terminal illness and dying with the dignity they deserve.
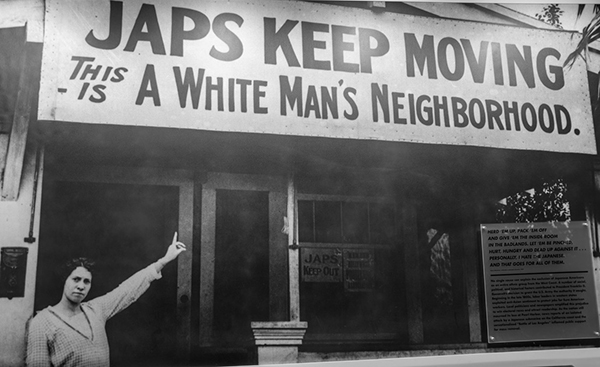
Systemic racism and social injustice permeate all aspects of society and are intertwined with the causes of health care disparities for African Americans, Hispanics and other diverse communities. And these same injustices are often perpetuated within the offices of the physicians and clinicians that many people of color are obligated to interact with.
As reported by MemoryCare.com, in California alone, 690,000 Americans are suffering from Alzheimer’s disease with the expectation that this number will increase by 21.7% by year 2025. Now, this astonishing number is a general fact and figure related to our population, but what’s even more astonishing is the fact that amongst Black Americans aged 70 or older, 21.3% are living with Alzheimer’s disease or another dementia.
That is almost one quarter of our Black senior population. Additionally, Black Americans are twice as likely to develop Alzheimer’s disease than their white counterparts, while Hispanic Americans are 1.5 times as likely to develop Alzheimer’s disease as their white counterparts.
Now, in a just, ethical and fair world designed to ensure that those at the highest clinical risk receive the most effective health care services, then Black and Hispanic Americans would report receiving high quality, competent and compassionate care, as well as experience positive patient outcomes. Unfortunately, we know for a fact that this is not true when it comes to health care delivery in America.
The American health care system is beset with inequalities that disproportionately impact people of color and other marginalized groups. And it is these inequalities that continue to contribute to gaps in health insurance coverage, uneven access to services and poorer health outcomes amongst certain populations.
Were you aware that when seeking clinical care for any disease, with Alzheimer’s being no different, almost 80% of Black Americans reported that they experience barriers to receiving quality care and support for Alzheimer’s disease?
In fact, more than 50% of Black Americans and 33% of Hispanic Americans state that they have experienced discrimination when seeking services for someone living with Alzheimer’s disease; while 34% of Asian Americans believe their race or ethnicity makes it more difficult to obtain care.
Furthermore, although people of all diverse populations continue to emphasize that cultural competency, cultural humility and cultural sensitivity are essential components for creating meaningful relationships, only 48% of the Black population and 59% of the Hispanic population feel confident they have access to providers who understand their ethnic or racial backgrounds and experiences.
Thus, when hearing these alarming statistics related to discrimination and health care related barriers, how likely do you think it is that a person or family member within our community, who is facing an uncurable disease like Alzheimer’s, is going to seek clinical support if they believe that provided support is not centered around delivering the necessary services in their best interest?
So, what can we do as a community to help develop culturally competent, inclusive care structures, and improving patient-community outcomes related to Alzheimer’s disease?
Community leaders who develop legislation surrounding health care equity and inclusion, must ensure Alzheimer’s disease and other dementias are part of the conversation.
We need policies created that address the disparities faced by those seeking a diagnosis and provide equitable and inclusive guidance and support to help families of color navigate our health care systems for access to tangible resources for them and their loved ones.
Primary care physicians, along with other health care professionals that serve a diverse population, must reach out to local organizations, such as the Alzheimer’s Association, to learn about the multitude of free training programs designed to enhance one’s understanding of how this disease presents, related risk factors for certain populations, the importance of an early diagnosis, and methods to improve engagement and deliver culturally competent and sensitive care.
Leaders of faith-based organizations must start talking about Alzheimer’s disease and begin collaborations with local organizations to help educate their members on the importance of an early diagnosis, proactive risk reduction actions related to brain health and healthy lifestyles, and available community resources.
In closing, we must begin to aid in the process of lifting associated stigmas that have existed in our community for far too long. As a people, we can no longer afford to allow our Alzheimer’s patients and caregivers to continue to suffer in silence.
Tia Delaney-Stewart is a registered nurse with more than 28 years of experience in the health care industry. She holds a master’s degree in nursing with an emphasis in education and is a certified clinical case manager.