By Marie Y. Lemelle
Contributing Writer
The global worry about the COVID-19 pandemic has redirected the focus of other life-threatening medical conditions and diseases. The world mourned for actor Chadwick Boseman, not only because he was 43 years old when he died from colon cancer, but because he was 39 when diagnosed with the disease.
Boseman’s death opened up a dialogue for thousands of people who avoided the reality about a disease that is considered to primarily affect individuals over 50 years old. Just as COVID-19 proved that younger people can be infected, colon cancer also can strike the younger generation.
The fact is one in five people diagnosed with colon cancer are between 20 and 54 years old. Colorectal cancer is the third most commonly diagnosed cancer in Black men and women. The four most common cancers (breast, prostate, colorectal and lung) account for more than one-half of all cancer cases among Blacks.
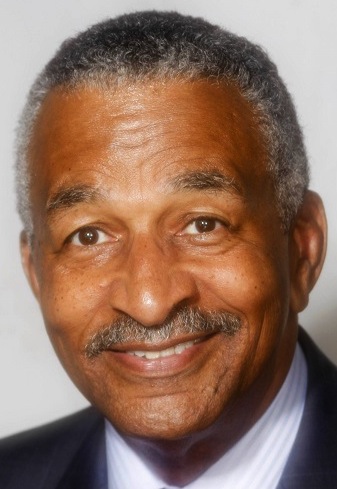
American Cancer Society Vice President for Prevention and Early Detection Dr. Durado Brooks authored the report, “COVID-19: Impact on Cancer Screening and Prevention,” which explores how the COVID-19 pandemic has led to unprecedented drops in breast, colorectal and cervical cancer screenings since the “stay safe at home” mandate was issued earlier this year.
To give a deeper perspective about colon cancer, I spoke with the Dr. Brooks who has worked for the American Cancer Society’s national headquarters since 2000. Dr. Books oversees the design, implementation and evaluation of cancer prevention and early detection programs at the national, state, and local levels to increase access to high quality prevention and screening, and to decrease cancer-related disparities.
ML: What is colon cancer?
DB: Most colorectal or colon cancers start as a growth, known as polyps, on the inner lining of the colon or rectum. Colorectal cancer means it started in the rectum and colon cancer means it started in the colon. They both are part of the large intestine, about five feet long, and part of the digestive system. If cancer forms in a polyp, it can grow into the wall of the colon or rectum over time.
ML: What are the symptoms and screening methods?
DB: Costs should not be the reason for not being screened. The Affordable Care Act requires health plans that started on or after Sept. 23, 2010 to cover colorectal cancer screening tests. In most cases there should be no out-of-pocket costs such as co-pays or deductibles for these tests.
If you experience any symptoms, like blood in stool, on the toilet paper, or in toilet bowl; notice changes in bowel movement habits that last more than seven days; have unexplained weight loss; and abdominal pain for more than a week; it is recommended to see your doctor immediately for tests.
Screenings include a colonoscopy, which is the way a doctor can view the entire length of the colon and rectum with a colonoscope, a flexible tube about the width of a finger with a light and small video camera on the end. The procedure should be done every 10 years.
Other screening methods are at-home stool collection test that is effective and inexpensive; virtual colonoscopy or CT colonography that enables the doctor to see inside of the colon and rectum for polyps or cancer. CT colonography must be done every five years; and the flexible sigmoidoscopy that looks at a certain part of the colon and rectum instead of looking at the entire length of the colon and rectum. The procedure should be scheduled every five years.
ML: Explain the four stages of colon cancer, treatment options and the survival rate.
DB: The stages of colon cancer is determined by how much cancer is in the body and what internal organs are affected. Early Stages 0 to 1, cancers have not yet penetrated the walls of the colon. Treatment can be removable of polyps or surgery to remove nearby lymph nodes. More than nine out of 10 will survive five year or longer.
Many Stage II colon cancers have grown through the wall of the colon, and maybe into nearby tissue, but they have not spread to the lymph nodes. Surgery to remove the section of the colon containing the cancer along with nearby lymph nodes may be the only treatment needed. A five-year survival rate of 87% is expected.
Stage III colon cancers have spread to nearby lymph nodes, but they have not yet spread to other parts of the body. Surgery to remove the section of the colon with the cancer along with nearby lymph nodes, followed by adjuvant chemo is the standard treatment for this stage. The overall survival rate at five years with treatment is between 43% and 83%.
Stage IV colon cancers have spread from the colon to distant organs and tissues. Colon cancer most often spreads to the liver, but it can also spread to other places like the lungs, brain, peritoneum or to distant lymph nodes. Treatment may include removal of sections containing cancer and nearby lymph nodes and chemo. Survival is about 14% beyond five years.
ML: Is it common for people in their 30s to get colon cancer, like Chadwick Boseman who was diagnosed at age 39?
DB: There are some generational connections like a pattern of cancer in the family which would place you in a higher risk group and screening should start as early as in your 20s. If you or a family member had pre-cancerous polyps removed, that is an indicator. The environment can also contribute to the early diagnosis.
Between 1990 and 2015, six out of every 100 were diagnosed with cancer. Now, it is 12 out of 100 patients. There has been a dramatic shift of variables that may contribute to colon cancer, such as obesity, type II diabetes, dietary intake of processed and red meat, tobacco use, antibiotics used indiscriminately and in food supply may harm the protective bacteria and possibly increase the growth of bad bacteria and hormonal impacts in livestock can contribute to the development.
ML: I had a colonoscopy in 2018 because both my mom and dad died of different forms of cancer – leukemia and Hopkins lymphoma, respectively. The colonoscopy was not an unpleasant experience because you are under anesthesia and there is no pain or long-term recovery. The knowledge of having a clean bill of health is the best news I could get from my digestive health doctor.
DB: It is important to talk about screenings with family and friends and encourage them to do the same. Finding and removing polyps early are a life-saving procedure.
Marie Y. Lemelle is the founder of www.platinumstarpr.com and a film producer. She can be reached at MarieLemelle@platinumstarpr.com. Follow her on Instagram @platinumstarpr.